Intelligent Automation for Hospital Capacity
AI-powered platform that reduces discharge delays and frees critical bed capacity
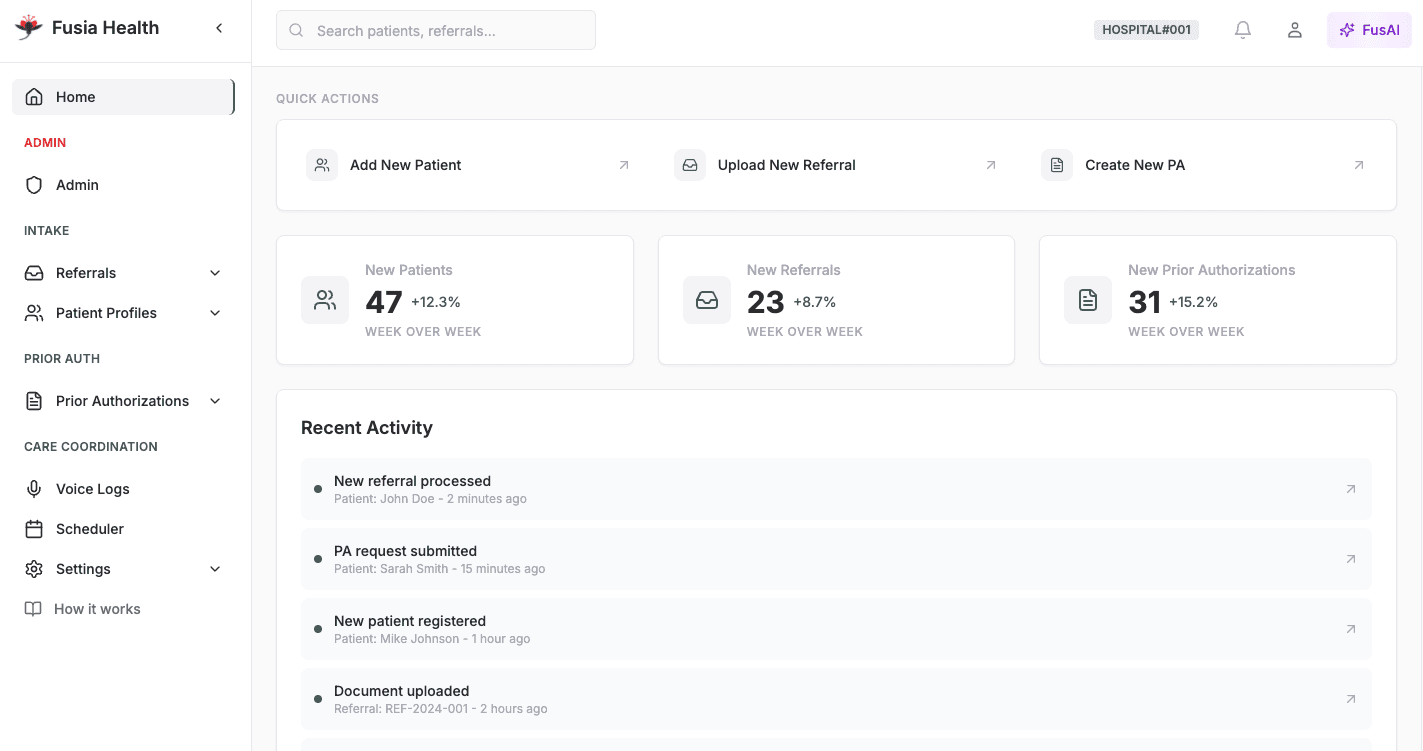
End-to-End Automation
Streamline your discharge workflows with intelligent automation that reduces delays and optimizes capacity.
Smart Intake
AI-powered referral processing that accelerates patient placement decisions.
Instant Authorization
Automated prior auth workflows that eliminate bottlenecks and reduce administrative burden.
Seamless Coordination
Real-time care orchestration that connects all stakeholders and ensures smooth transitions.